Total shoulder arthroplasty is considered one of the greatest achievements in orthopedic surgery. This procedure involves replacing the damaged portions of the shoulder joint with specially designed implants that are both long-lasting and biocompatible.
It is a highly effective surgical procedure, primarily offering significant pain relief and improving shoulder mobility that is often restricted due to arthritis. In addition to reducing stiffness, total shoulder arthroplasty helps restore strength and function, enabling patients to resume their daily routines with greater ease.
Over time, the smooth cartilage that covers the ends of the bones in the shoulder joint gradually wears away. As the cartilage thins, the protective space between the bones decreases and the bones begin to rub directly against each other during movement. This friction causes the joint surfaces to become rough, and bone spurs (osteophytes) can form along the edges of the joint. The direct bone contact and irregular surfaces cause pain, stiffness, and a grinding or clicking feeling in the shoulder.
Total shoulder arthroplasty is often recommended to manage such conditions, including:
The most common reason for recommending total shoulder arthroplasty (shoulder replacement surgery) is severe, persistent shoulder pain from arthritis that doesn’t respond to non-surgical treatments like pain medication or steroid injections. This type of arthritis involves the loss of protective cartilage, leading to bone-on-bone friction that causes pain, stiffness, and limited movement. Surgical intervention is recommended in these cases to relieve pain and restore function, as timely surgery can help prevent further joint damage.
A standard two-view X-ray is typically the initial step for assessing the shoulder joint’s condition. In certain cases, additional imaging tests such as a CT scan or MRI may be required to accurately assess the severity and progression of arthritis. A CT scan provides superior imaging of bone, making it ideal for assessing issues like glenoid bone loss and fractures, while MRI is excellent for evaluating soft tissues like the rotator cuff and labrum.
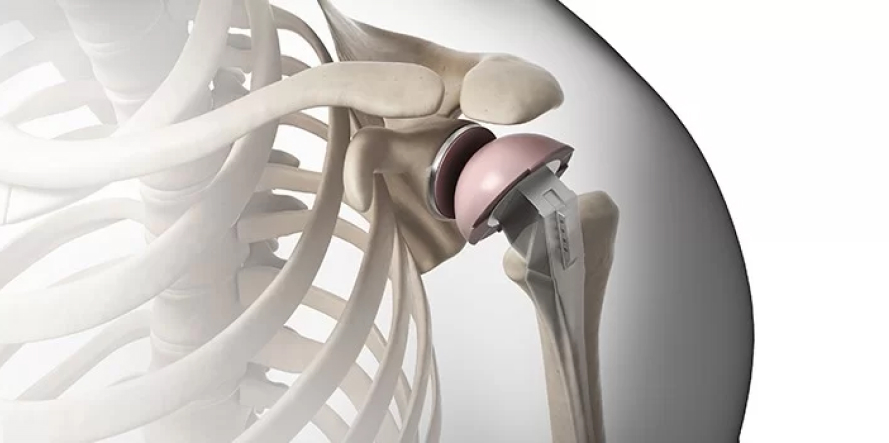
In total shoulder arthroplasty, damaged joint surfaces are carefully removed and the surrounding area is cleaned. The remaining healthy bone is then shaped to accommodate the prosthetic components. Once the implants are positioned, the surgeon ensures proper alignment and joint mobility.
The implants, made from biocompatible metal or ceramic materials, are designed to function safely within the human body. The procedure is carried out under general anesthesia and typically lasts about 60-80 minutes.
There are two main types of total shoulder arthroplasty:
Total shoulder arthroplasty (TSA) complications are uncommon and often manageable, with potential issues including joint stiffness, instability, and nerve irritation. In the hands of skilled and experienced shoulder orthopedic surgeons, the complication rates are extremely low.
Following a total shoulder arthroplasty, patients begin a customized rehabilitation plan designed to help them safely return to daily activities. The primary focus is to gradually restore full range of motion and rebuild strength, ultimately supporting a return to normal daily activities.
Basic self-care and hygiene tasks can typically be performed soon after surgery, as prolonged immobilization is not required. In fact, early and guided movement is encouraged, always under the close supervision of the treating orthopedic surgeon and physiotherapist.
For an individual evaluation based on the stage of your condition and for the appropriate choice of shoulder arthroplasty according to your symptoms, please, consult the orthopedic surgeon, Dr. Panagiotis Pantos.
Fill in your details below and we will contact you immediately!
WIN THE
MATCH POINT IN THE RACE
OF YOUR HEALTH!